Bone Marrow Transplant in India
Bone marrow transplant (BMT) is a life-saving procedure for patients suffering from blood-related diseases such as leukemia, thalassemia, lymphoma, and aplastic anemia. The cost of a bone marrow transplant in India ranges from USD 18,000 to USD 35,000. With the rising cost of healthcare in Western countries, many international patients are now turning to India for affordable and high-quality treatment options.
What Is a Bone Marrow Transplant and Who Needs It?
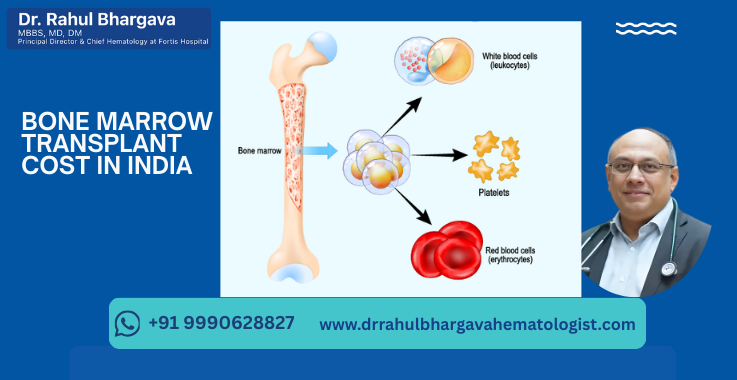
A bone marrow transplant is a medical procedure that involves replacing damaged or destroyed bone marrow with healthy stem cells. These stem cells may come from the patient’s own body or a donor. The goal is to help the body produce healthy blood cells, including white blood cells, red blood cells, and platelets.
BMT can be curative or life-extending for a variety of both malignant (cancerous) and non-malignant diseases. Common conditions treated with BMT include:
- Leukemias: Acute and chronic leukemias are among the most frequent indications for allogeneic BMT. A transplant can replace the diseased marrow with healthy cells to induce long-term remission.
- Lymphomas: Both Hodgkin and Non-Hodgkin lymphomas, especially relapsed cases, may be treated with BMT (often autologous transplant) to rebuild the immune system after high-dose chemotherapy.
- Multiple Myeloma: Autologous stem cell transplant is a standard therapy for multiple myeloma, significantly extending remission times.
- Myelodysplastic Syndromes (MDS) and Myeloproliferative Disorders: Conditions like myelodysplasia or myelofibrosis can be cured with allogeneic transplants by introducing healthy stem cells.
- Aplastic Anemia: Severe aplastic anemia (bone marrow failure) often necessitates an allogeneic transplant to provide the patient with a new source of blood formation.
- Thalassemia & Sickle Cell Disease: These inherited blood disorders can be cured with a bone marrow (stem cell) transplant, typically from a matched sibling donor.
- Immune Deficiency Disorders: Certain immunodeficiencies (like SCID) or genetic metabolic disorders are treated with BMT to establish a functioning immune system.
Types of Bone Marrow Transplants Offered in India
Understanding the different kinds of bone marrow transplants enables patients to choose the most suitable option based on their individual medical needs and budget.
- Autologous Bone Marrow Transplant: In an autologous transplant, doctors use the patient’s own stem cells. These cells are collected, stored, and re-infused after intensive chemotherapy. This type of transplant is commonly used for patients with lymphoma or multiple myeloma.
- Allogeneic Bone Marrow Transplant: Allogeneic transplants use stem cells from a donor. The donor may be a sibling, a relative, or an unrelated person found through a donor registry. This method is often used for conditions like leukemia, thalassemia, and aplastic anemia.
- Haploidentical Bone Marrow Transplant: Haploidentical transplants utilize a half-matched donor, typically a parent or sibling. This type of transplant is increasingly popular in India because it increases donor availability and reduces wait time for treatment.
Bone Marrow Transplant Cost in India
One of the many advantages of choosing India for a bone marrow transplant is the significantly lower cost compared to many Western countries. The average price of BMT in India ranges from approximately USD 15,000 to USD 40,000 (INR 12–33 lakhs), depending on the type of transplant and its complexity. By contrast, the same procedure can cost anywhere from USD 100,000 to USD 200,000 or more in the United States or the United Kingdom. This cost difference has made India a leading destination for patients worldwide seeking affordable bone marrow transplants (BMT).
Cost Breakdown by Transplant Type
The cost of BMT varies by the type of transplant. Autologous transplants are generally the least expensive, while allogeneic transplants cost more due to donor-related expenses. Haploidentical transplants can be slightly more than a fully matched allogeneic transplant because of additional protocols to manage partial matching. Below is a breakdown of typical cost ranges in India for each transplant type:
Autologous Transplant: USD 18,000–20,000. Autologous BMT is cheaper since there are no donor search or harvesting costs – the patient is their own donor. The main expenses are hospitalization, chemotherapy, and re-infusion of stem cells.
Allogeneic Transplant (Related Donor): USD 22,000–25,000. Allogeneic costs are higher due to donor testing (HLA typing), donor stem cell collection, and graft processing. If the donor is a sibling or relative, costs include their medical evaluation and collection procedure.
Haploidentical Transplant: USD 30,000–35,000. Haploidentical (half-match) transplants often incur additional costs for specialized protocols to manage partial matching and reduce complications.
Unrelated Donor Transplant: USD 50,000–70,000. If a matched donor is not available in the family, an unrelated donor transplant may be done through international registries. This significantly increases cost due to registry search fees and donor procurement expenses.
Detailed Cost Breakdown for Bone Marrow Transplant in India
A bone marrow transplant involves several stages, each with its own associated costs. Understanding the cost structure helps international patients plan their budgets and avoid surprises.
|
Cost Component |
Estimated Cost (USD) |
|
Pre-transplant investigations |
1,000 – 1,500 |
|
Chemotherapy and conditioning therapy |
1,500 – 2,500 |
|
Stem cell harvesting |
1,000 – 1,500 |
|
ICU & hospital stay |
250 – 400 per day |
|
Medications and supportive care |
4,000 – 6,000 |
|
Donor matching and HLA typing |
150 – 250 |
|
Total Estimated Cost |
18,000 – 35,000 |
Comparing Bone Marrow Transplant Costs: India vs Other Countries
India is one of the most cost-effective countries for bone marrow transplant treatment, especially for international patients. Patients traveling to India can save up to 80% on bone marrow transplant costs without compromising on quality. Here’s how the cost compares globally:
|
Country |
Average BMT Cost (USD) |
|
India |
USD 15,000 – USD 45,000 |
|
United States |
USD 200,000 – USD 400,000 |
|
United Kingdom |
USD 150,000 – USD 250,000 |
|
Singapore |
USD 120,000 – USD 180,000 |
|
Turkey |
USD 60,000 – USD 90,000 |
Factors Affecting the Cost of Bone Marrow Transplant in India
While India is cost-effective, the final cost can still vary depending on a few critical factors. These need to be considered when planning treatment.
- Type of Transplant: Allogeneic and haploidentical procedures are costlier than autologous.
- Hospital Chosen: Premium hospitals in metro cities charge more than smaller institutions.
- Doctor’s Expertise: Highly experienced specialists may charge more for consultation and surgery.
- Complications: Pre-existing infections or complications during recovery can add to the cost.
- Length of Stay: Prolonged hospitalization increases overall expenses.
- Use of Donor Registry: If no family match is found, unrelated donor registry fees apply.
What is Included in the Cost of BMT?
When budgeting for a bone marrow transplant, it’s crucial to understand what the quoted cost covers. Generally, the following are included in most BMT cost estimates in India:
- Hospital Stay and Procedure: The cost covers both the surgery or procedure itself and hospitalization for the duration of the transplant. BMT often requires a protective isolation room for 3–4 weeks post-transplant, which is accounted for in the package.
- Pre-Transplant Investigations: All necessary pre-operative tests (blood tests, HLA typing for donor matching, scans, etc.) are usually included. This ensures the patient is fit for transplant and the donor (if any) is compatible.
- Medication and Consumables: High-dose chemotherapy drugs, IV fluids, transfusions, and supportive medications are part of the cost during the hospital stay. Consumables, such as catheters and infusion pumps, as well as personal protective equipment for infection control, are also included.
- Donor Workup & Harvest (for Allogeneic): If a family donor is involved, their testing and stem cell harvest procedure costs are generally included in the package. (Do verify this – some hospitals charge the donor’s hospitalization separately, but many include it.)
- In-Patient Meals and Nursing Care: Patients (and often one attendant) are provided meals. The cost of round-the-clock nursing, intensive care if needed, physiotherapy, and other related services is also included.
- Post-Transplant Monitoring (In-Hospital): Daily lab tests to track engraftment, any needed scans, and basic follow-up within the hospitalization period are covered.
On the other hand, costs that are usually not included (to be prepared for separately) include:
- Post-Discharge Medications and Follow-ups: Following discharge, patients will require regular follow-up visits, blood tests, and medication (e.g., immunosuppressants) for several months. These outpatient costs are typically extra. For instance, immunosuppressant injections can cost INR 20,000–25,000 if required, and regular medicines and check-ups in the first 3–6 months may add INR 50,000 or more (which is minor compared to the transplant but should be budgeted for).
- Donor Registry Fee (if applicable): If using an unrelated donor or cord blood unit from a registry, the procurement fee is additional. This can be substantial (e.g., USD 20,000 or more per unit from an international registry) and is charged separately.
- Accommodation Outside Hospital: The cost of staying in India before admission and after discharge (in a guesthouse or hotel) is not included. Many packages, however, will help arrange nearby accommodations at discounted rates. Patients often need to stay nearby for a few weeks after discharge.
- Travel Expenses: Airfare to India, domestic travel, and medical visa fees are borne by the patient (though hospitals often provide invitation letters and airport transfers).
- Complications Beyond Standard Care: If a severe complication occurs (e.g., extended ICU care beyond the package terms, retransplant, prolonged ventilation), the associated costs may exceed the package terms. It’s wise to have an emergency fund or insurance for unexpected events.
Why International Patients Choose India for Bone Marrow Transplant
India has steadily become a preferred destination for medical tourism, particularly for bone marrow transplants, due to its combination of affordability, expertise, and advanced infrastructure.
- Cost-Effective Treatment: India offers the most affordable bone marrow transplant costs in the world, making it a preferred destination for medical tourism.
- Highly Skilled Specialists: India boasts some of the world’s top hematologists and oncologists, such as Dr. Rahul Bhargava.
- Advanced Medical Technology: Indian hospitals are equipped with the latest technologies, such as high-dose chemotherapy, stem cell harvesting, and bone marrow cryopreservation.
- Faster Treatment Timelines: Patients receive quick consultations and faster surgical scheduling compared to the long waiting lists found in Western countries.
- English-Speaking Medical Staff: Doctors and hospital staff in India speak fluent English, which simplifies communication for international patients.
- Comprehensive Support for International Patients: From visa assistance to post-treatment follow-up, Indian hospitals offer comprehensive support for international patients.
BMT Success Rate in India
India’s leading transplant centers have achieved success and survival rates comparable to the best centers globally. The success rate can be defined in various ways (engraftment success, disease-free survival, overall survival), but in general:
- Overall Survival: The overall survival rate for BMT patients in India is around 70–80%, considering all transplant types and diseases. This means that the majority of patients achieve long-term survival or a cure, although the outcome varies by condition.
- Autologous vs. Allogeneic: Autologous transplants have a slightly higher immediate success rate (since there’s no risk of rejection or GVHD) – in India, autologous BMT success is ~80–90% for eligible patients. Allogeneic transplants have success rates of around 70–85% in India, depending on donor match and disease status. These figures are comparable to international standards, reflecting India’s medical excellence.
- Pediatric Success: Notably, children often do very well – pediatric BMT survival in India can reach 80–90% in many cases, especially for non-malignant conditions (like thalassemia or immune deficiencies) when done early
- Disease-Specific Outcomes: Success also depends on the underlying disease. For example, transplants for thalassemia in children have high cure rates (~90% with a sibling donor). In comparison, advanced leukemia transplants might have lower long-term disease-free survival (50–70%, varying by leukemia subtype and risk factors). Early-stage transplants generally have better outcomes.
- Improvements Over Time: Success rates in India have improved significantly over the last few years, thanks to better infection control, advanced therapies, and expanded donor options. Studies show that transplant success in India has risen from ~50-60% in the early 2000s to around 70% in recent years for allogeneic cases. Some leading hospitals, such as the FMRI, report a 5-year survival rate of over 80% in specific patient groups.
Recovery After Bone Marrow Transplant in India
Recovery from a BMT procedure is a gradual process, requiring patience and adherence to medical advice. Here’s what to expect in terms of recovery timeline and care:
- Initial Hospital Recovery: After the transplant (day “0”), patients remain in the hospital until the transplanted stem cells engraft (start producing new blood cells). It takes about 2 to 4 weeks. Most patients stay in a protective isolation room during this period to prevent infections. You may feel very weak, experience side effects like nausea or mouth sores, and require blood transfusions. From Day 14 to Day 30, as counts recover, doctors assess if it’s safe to discharge.
- Time to Discharge: Many people are well enough to leave the hospital within 1 to 2 months post-transplant. In fact, discharge often occurs between 3 to 6 weeks post-transplant if there are no significant complications. Autologous transplant patients tend to have shorter hospital stays (~3 weeks) compared to allogeneic transplant patients (4–6 weeks due to graft monitoring and GVHD surveillance).
- Immediate Post-Discharge: Even after leaving the hospital, close monitoring continues. For the first 3 months, patients need to stay near the transplant center for regular follow-ups (often weekly). You’ll be on medications to prevent infections and GVHD (for allogeneic cases). During this time, the risk of infection remains high, so taking precautions (such as wearing masks, avoiding crowds, and maintaining a safe diet) is necessary. Hospitals in India typically schedule a formal evaluation at approximately Days 30, 60, and 100 post-transplant.
- 3 to 6 Months: The immune system remains weak for up to 6 months after transplant. By three months, many patients experience significant improvement, and their blood counts stabilize; however, they must continue infection prophylaxis and avoid live vaccines. If allogeneic, any signs of graft-versus-host disease (GVHD) will be closely monitored and managed. By six months, if there are no complications, patients can often resume more normal activities gradually.
- 1 Year and Beyond: It can take a year or more for complete immune reconstitution to occur. For some, it may take even 2 years to feel fully recovered. Routine vaccinations (reimmunization) are typically initiated around 1 year post-transplant. Follow-up visits become less frequent (perhaps monthly or quarterly) after the first year if all is well.
- Success and Relapse: If the transplant is successful, the new bone marrow will produce healthy cells, and the underlying disease will be in remission. Doctors typically conduct a detailed assessment at 100 days, 6 months, and 1 year (including bone marrow biopsies and chimerism tests to confirm donor cells, among other tests). Relapse, if it occurs, typically happens within the first 2 years. Surviving disease-free past 2–3 years is a very good sign.
Recovery Tips
During recovery, patients should maintain a nutritious diet, adhere to medication schedules, perform light exercises as advised (to regain strength), and immediately report any signs of infection or GVHD to doctors. Indian hospitals usually provide a detailed discharge summary with do’s and don’ts. International patients often have the option for telemedicine follow-ups once they return home; however, it’s recommended that they stay in India for at least three months post-transplant for optimal monitoring.
Remember, every patient’s recovery is unique – some may bounce back in a few months, while others take longer. The key is regular follow-up and not getting discouraged by temporary setbacks. With today’s protocols, most BMT patients in India go on to lead healthy lives after transplant once recovery is complete.
Medical Visa for Bone Marrow Transplant in India
India offers a dedicated medical visa category for patients seeking treatment in Indian hospitals. Most hospitals assist with the application process to ensure a smooth travel experience.
- A visa invitation letter from an Indian hospital
- Recent medical reports
- Passport copy
- Proof of ability to afford treatment
Visa approvals are generally processed within 72 hours.
Bone Marrow Transplant at Fortis Memorial Research Institute, Gurgaon
Fortis Memorial Research Institute (FMRI) in Gurgaon is one of India’s most advanced and trusted hospitals, particularly for international patients seeking complex procedures such as bone marrow transplants. Equipped with cutting-edge technology and dedicated transplant units, FMRI offers world-class care with the highest safety and hygiene standards. The hospital is NABH- and JCI-accredited and is well-known for its personalized care and infection-controlled environment, especially in oncology and hematology services.
Key Services for International Patients at FMRI:
- Dedicated Bone Marrow Transplant (BMT) Unit with HEPA-filtered rooms
- Pre-transplant counseling and donor-matching support
- High-end diagnostic labs and radiology for quick assessments
- Personalized treatment plans following international BMT protocols
- 24/7 ICU and emergency care for high-risk transplant patients
- In-house blood bank and cryopreservation facilities
- Infection control and a sterile environment for post-transplant recovery
- Multilingual international patient coordinators and visa assistance
- Video consultations and post-treatment follow-ups via telemedicine
Frequently Asked Questions
Yes, Indian hospitals follow global safety standards and protocols. Thousands of successful procedures are done every year.
Most international patients stay for 2 to 3 months, which includes preparation, transplant, and early recovery.
If a family donor isn’t available, Fortis Memorial Research Institute, Gurgaon, can help you access donor registries or perform haploidentical transplants.
You will need your passport, medical reports, and visa documents. The hospital will guide you through the process.
Yes, Dr. Rahul Bhargava offers post-treatment consultations via video or phone to international patients.
