Hemoglobinopathies
Hemoglobinopathies
Contact Us
Related Videos :
Frequently Asked Questions (FAQ) :
Some hemoglobinopathies, such as sickle cell disease and beta-thalassemia major, can be cured with a bone marrow transplant or gene therapy. However, not all patients are candidates for these treatments.
Hemoglobinopathies are inherited in an autosomal recessive pattern, meaning both parents must carry a defective gene to pass the disorder to their child.
Yes, prenatal genetic testing can detect hemoglobinopathies in a fetus, allowing parents to make informed decisions about the pregnancy and early care.
Long-term complications can include organ damage, growth delays, bone deformities, and increased risk of infections. Regular monitoring and appropriate treatment are essential to managing these complications.
Patients with hemoglobinopathies should maintain a healthy diet, avoid infections, and stay hydrated. Regular check-ups and adherence to treatment plans are also crucial for managing the condition.
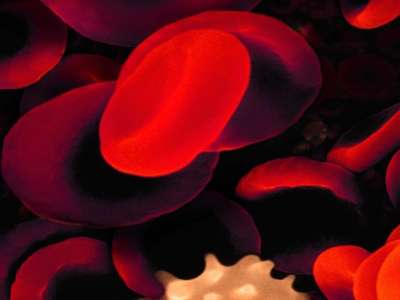
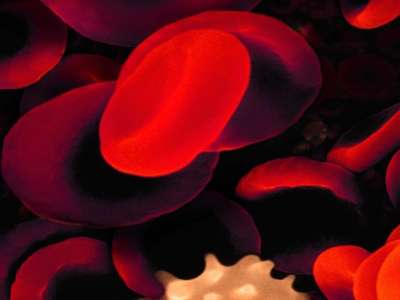
About Hemoglobinopathies
Hemoglobinopathies are a group of inherited blood disorders characterized by abnormalities in the hemoglobin molecule, the protein in red blood cells responsible for carrying oxygen throughout the body. These disorders result from mutations in the genes that encode hemoglobin, leading to altered structure or function of the hemoglobin molecule. Common hemoglobinopathies include sickle cell disease, thalassemia, and other rare variants. Dr. Rahul Bhargava, a leading hematologist, offers specialized care for patients with hemoglobinopathies, providing comprehensive diagnosis and treatment options tailored to each patient’s needs.
Causes of Hemoglobinopathies
Hemoglobinopathies are genetic disorders passed down from parents to children. They occur due to mutations in the genes responsible for producing hemoglobin:
- Genetic Mutations: Mutations in the HBB, HBA, or other related genes lead to the production of abnormal hemoglobin. These mutations are typically inherited in an autosomal recessive manner, meaning both parents must carry the defective gene for their child to inherit the disorder.
- Inheritance Patterns: If both parents carry a hemoglobinopathy trait, there is a 25% chance with each pregnancy that the child will inherit the disorder, a 50% chance that the child will be a carrier, and a 25% chance that the child will be unaffected.
- Geographic and Ethnic Factors: Hemoglobinopathies are more common in certain populations, particularly those of African, Mediterranean, Middle Eastern, and Southeast Asian descent.
Types of Hemoglobinopathies
Hemoglobinopathies are primarily categorized based on the type of genetic mutation and the effect on hemoglobin function:
- Sickle Cell Disease (SCD): This is the most well-known hemoglobinopathy, caused by a mutation in the HBB gene, leading to the production of abnormal hemoglobin S. The red blood cells become sickle-shaped, leading to blockages in blood flow and various complications.
- Thalassemias: These are a group of inherited blood disorders caused by mutations that affect the production of hemoglobin. The two main types are:
- Hemoglobin C, D, and E Variants: These are less common forms of hemoglobinopathies where different mutations lead to abnormal hemoglobin variants with varying clinical implications.
Symptoms of Hemoglobinopathies
The symptoms of hemoglobinopathies can vary widely depending on the type and severity of the disorder:
- Anemia: Most hemoglobinopathies cause varying degrees of anemia, leading to symptoms such as fatigue, weakness, and pale skin.
- Jaundice: Due to the rapid breakdown of abnormal red blood cells, patients may develop jaundice, characterized by yellowing of the skin and eyes.
- Pain Episodes: In conditions like sickle cell disease, patients may experience painful episodes known as vaso-occlusive crises, caused by blockages in blood flow.
- Growth and Developmental Delays: Severe forms of thalassemia and sickle cell disease can lead to delayed growth and development in children.
- Organ Damage: Over time, hemoglobinopathies can cause damage to vital organs, including the spleen, liver, heart, and kidneys, due to chronic anemia and reduced oxygen delivery.
- Bone Deformities: In thalassemia, bone marrow expansion to compensate for anemia can lead to skeletal abnormalities.
Diagnosis of Hemoglobinopathies
Diagnosing hemoglobinopathies involves several steps, including:
- Blood Tests: A complete blood count (CBC) and hemoglobin electrophoresis are commonly used to identify abnormal hemoglobin variants and assess the severity of anemia.
- Genetic Testing: Molecular genetic tests can identify specific mutations in the hemoglobin genes, confirming the diagnosis and determining the exact type of hemoglobinopathy.
- Newborn Screening: In many countries, newborn screening programs detect hemoglobinopathies shortly after birth, allowing for early intervention and management.
- Prenatal Testing: For families at risk, prenatal genetic testing can determine if a fetus has inherited a hemoglobinopathy.
Treatment of Hemoglobinopathies
The treatment approach for hemoglobinopathies varies depending on the type and severity of the disorder:
- Blood Transfusions: Regular blood transfusions are often necessary for patients with severe anemia, particularly those with beta-thalassemia major.
- Iron Chelation Therapy: Patients receiving frequent blood transfusions are at risk of iron overload, which requires chelation therapy to remove excess iron from the body.
- Bone Marrow Transplant (BMT): BMT is currently the only curative treatment for some hemoglobinopathies, particularly sickle cell disease and severe thalassemia. It involves replacing the patient’s bone marrow with healthy marrow from a compatible donor.
- Hydroxyurea Therapy: This medication is commonly used in sickle cell disease to reduce the frequency of pain episodes and other complications.
- Gene Therapy: Emerging gene therapy techniques offer the potential for curing hemoglobinopathies by correcting the underlying genetic defects.
- Supportive Care: Managing symptoms and preventing complications through regular monitoring, pain management, and treating infections is a critical aspect of care.
Cost of Treatment and Stay in India
The cost of treatment for hemoglobinopathies in India is generally lower compared to many Western countries, making it an attractive option for medical tourism. The overall cost can vary based on the type of treatment required, the severity of the condition, and the healthcare facility chosen.
- Blood Transfusions: Regular transfusions may cost around $100–$500 per session (INR 8,000–40,000).
- Iron Chelation Therapy: The cost of medication for iron chelation may range from $200–$1,000 per month (INR 15,000–75,000).
- Bone Marrow Transplant (BMT): The cost of a bone marrow transplant can range from $15,000 to $30,000 (INR 12,00,000–24,00,000).
- Gene Therapy: Emerging gene therapies may cost around $100,000–$250,000 (INR 75,00,000–1,87,00,000) depending on the specific procedure.
- Hydroxyurea Therapy: The cost for hydroxyurea medication typically ranges from $50–$200 per month (INR 4,000–15,000).
Stay and Accommodation: For international patients, the cost of stay in India can vary, with average hotel prices ranging from $30 to $150 per night (INR 2,500–12,000), depending on the location and quality of accommodation.
Overall, the total cost for treatment, including hospital stay and medication, may range from $5,000 to $40,000 (INR 4,00,000–32,00,000), depending on the complexity of the case and the required treatment plan.